
Baie eerstes vir die CTAFC
Die Cape Town AF Centre met Dr Razeen Gopal aan die stuur, word wêreldwyd hoof aangeslaan en dié sentrum word byna sonder uitsondering deur vervaardigers van nuwe mediese harttegnolgie gekies

Die Cape Town AF Centre met Dr Razeen Gopal aan die stuur, word wêreldwyd hoof aangeslaan en dié sentrum word byna sonder uitsondering deur vervaardigers van nuwe mediese harttegnolgie gekies
The morning of your ablation a CT or MRI of your left atrium is performed so that we can import this into our EP Systems.

A pacemaker is an implanted device that monitors your heartbeat and prevents your heart from beating too slowly.

Hartversaking beteken letterlik dat jou hart versaak en nie voldoende bloed uit jou hart pomp sodat jou liggaam en brein goed kan funksioneer nie.

Arrhythmias include atrial fibrillation, atrial flutter, AVNRT, Wolff-Parkinson-White syndome and ventricular tachycardias.

THE CAPE TOWN AF CENTRE IS BASED AT PANORAMA MEDICLINIC HEART UNIT.

Waarom klop ’n mens se hart soms te vinnig, te stadig of onreëlmatig? Wanneer is dit gevaarlik? Kan of moet dit behandel word? Hoe word dit behandel?
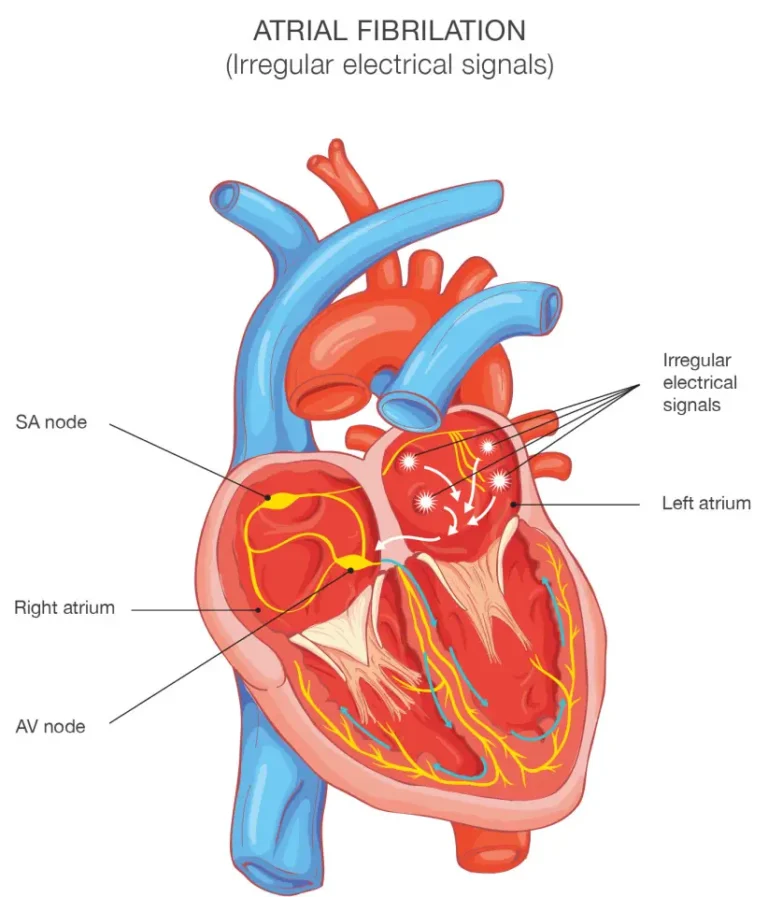
Although we treat all forms of cardiac arrhythmia, atrial fibrillation is the commonest and most confusing for patients, so here is some more information.

A rapid and irregular pulse is the commonest sign of AF and is usually the way in which it is discovered in people without any symptoms.

The most important thing is to confirm whether you do have AF or not. This is done by recording the electrical activity of the heart during your symptoms (or when