Catheter ablation (using wires passed up from the leg to deliver energy to cause electrical conduction block) seeks to modify the electrical properties of the atria so that they are less likely to fibrillate in the future.
There are a number of different techniques used at the moment which are evolving rapidly. The latest technique involve electroporation (also known as pulsefield ablation) or cryo-ablation for atrial fibrillation and Radio-frequency (RF) ablation for AF and other arrhythmias.
Because of this the results of catheter ablation have improved rapidly and now most experienced centres will be able to offer patients with paroxysmal (intermittent) AF with no structural heart abnormalities an 80% chance of eliminating AF without drugs.
Some centres can also achieve this 80% success rate for patients with permanent AF. In order to achieve these results up to 50% of patients need to have repeat procedures.
Results published by some centres can be confusing because some do not even follow patients up in person let alone do Holter monitoring (a continuous recording of the ECG lasting from 24 hours to 7 days exclude asymptomatic AF (AF without symptoms). Other centres do not make it clear how many patients require repeat procedures or the help of antiarrhythmic drugs to keep them in normal sinus rhythm.
BENEFITS
Catheter ablation can restore normal sinus rhythm and avoid the need for drugs. There is early evidence that mortality may be reduced by catheter ablation but this is yet to be confirmed.
There is also early evidence that catheter ablation of patients with AF and heart failure can have their heart function improved by restoration of sinus rhythm by catheter ablation.
SUCCESS RATES
70% to 80% off drugs after multiple procedures. This is likely to be lower if patients has structural heart disease (e.g. valve disease)
COMPLICATIONS
Complications occur in about 1 to 5% of patients.
The most common complication is pericardial effusion (blood leaking out of the heart) which may need draining with a needle or operation. This is the result of the anticoagulation (blood thinning) drugs required to be given during the procedure. The main reason for this is to avoid clots forming on the catheters. If clots do form then they may be dislodged and travel to the arteries feeding the brain. This could cause stroke.
Other complications include bruising in the legs, and chest pain. Chest pain can be relieved by pain killers during the procedure but can persist for a few weeks because of the inflammation from the procedure. Simple pain killers can be used to alleviate this until it settles.
Another complication is narrowing of the pulmonary veins. These are the veins that drain blood from the lungs into the heart and is related to how far into the veins energy is applied and how much energy is applied. This does not appear to have been a problem at our centre since we adopted a policy of only delivering very low energies near the veins.
The rarest but most concerning complication is atrio-oesophageal fistula. This has happened 14 times in world experience so far. It is a complication which occurs 2 weeks or so after the ablation when a hole forms between the atrium and the oesophagus (gullet).
The first symptoms are stroke-like symptoms followed by vomiting blood and death. Only 2 patients have survived this complication. No one knows what causes this complication but it may be related to delivering a lot of energy particularly in the back of the atrium. Many centres deliver 100 watts into the left atrium to achieve their results. We only deliver 30 watts in the atrium and 20watts near the veins.
Types of catheter ablation
1. Electroporation / Pulse Field Ablation for AF
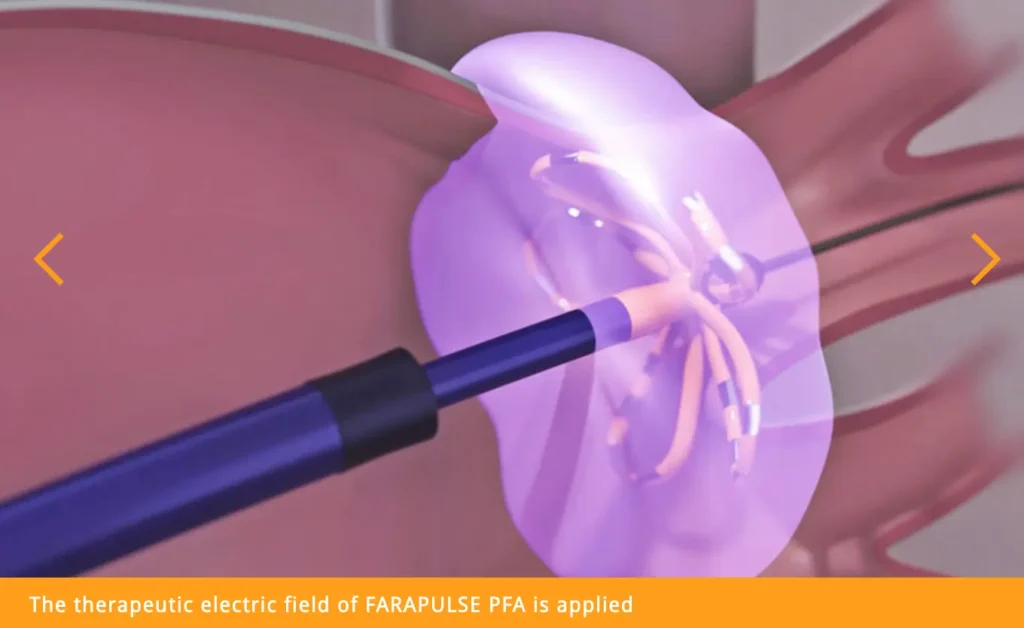
Pulse Field ablation uses electrical impulses at a specific frequency to target only heart cells, with no damage to any other cells.
Pulse field ablation is safe and effective and currently most often used at the CTAFC since it was introduced to the Emerging markets (Africa and the Middle East) at this centre.
Read more about Pulse Field ablation here and watch the video.
2. Cryoballoon ablation for AF

Cryoablation uses cold energy (freezing) delivered through an inflatable balloon to create scar tissue to interrupt unwanted electrical pathways in the heart.
The cryo balloon comprises of a balloon on the end of a catheter which is inflated in the left atrium and then jammed in each of the pulmonary veins in turn. When the balloon is in the vein it is then frozen by passing gas through the catheter.
Where the balloon is in contact with the vein it causes freezing of the tissue and cell death. This renders the tissue electrically inert. The damage caused by cryoablation is less traumatic than RF and therefore it is less likely to cause damage to the veins. Unsubstantiated claims that cryo is less likely to cause stroke have never been proven.
In addition cryoablation can be associated with damage to the nerve that stimulates the diaphragm (the phrenic nerve) but this does not usually cause symptoms and in all published reports has recovered within 12 months.
The potential problem with cryoablation is that it only works if the balloon is in contact with the tissue and while the balloon is perfectly circular, the pulmonary veins are not. Therefore it is not uncommon for operators need to use an additional catheter at the end of the procedure (either cryo or RF) to close the gaps left by the balloon.
Cryoablation is used by many centres because it is felt to be faster and safer than RF ablation for AF, and good results have been published in non-randomised studies.
Approximately 75% of patients with paroxysmal (intermittent) AF don’t need any anti-arrhythmia medication within one year post-procedure, while 60% of patients with persistent AF recover from AF after a series of ablations. These success rates achieved at Dr Gopal’s unit compare well with the very best internationally.
3. CIRCULAR ABLATION CATHETERS for AF
This is a system where the catheter is not bent by a puller wire inside the catheter and is floppy. The tip of the catheter has metal in it and strong magnetic fields are used to bend the catheter.
The catheter can be advanced using a motorised drive unit placed on the patient’s groin which allows the operator to control catheter movement from outside the catheter lab and away from x-rays. The advantage to this system is that perforation by the catheter seems very unlikely because the catheter is so floppy that it cannot be pushed through the heart wall.
Whether this is really an issue is not clear because although blood leaking out of the heart is a common complication of AF ablation this is rarely results from catheter perforation and may be related to the transseptal puncture required to access the left atrium with any technology, or as the result of an RF lesion causing perforation. Nevertheless the magnetic system allows precise manipulation of the catheter around the heart and therefore the potential for very accurate RF lesion placement.
One of the technical challenges has been to produce a cool-flow catheter that is sufficiently floppy to allow the magnets to manipulate it.
Cool flow describes a catheter where saline is passed down the central lumen of the catheter and sprayed out of the end over the catheter tip. This is generally used in AF ablation because we believe it may reduce the chances of blood clot formation on the catheter tip and therefore stroke (unproven in randomised trials).
The difficulty of maintaining the integrity of a central lumen used for the saline and making the catheter floppy has now been overcome and this catheter is now in use. This may however explain why magnetic navigation has been in clinical use for almost 10 years and no data demonstrating that it is effective for AF ablation have been published.
There are concerns that the magnets may not be able to bend the catheter with sufficient force to produce adequate RF lesions but this again is not substantiated.
Read more about this technique: https://capetownafcentre.com/eerste-multi-elektrode-ablasie-in-afrika-suksesvol-gedoen/
4. RADIOFREQUENCY CATHETER ABLATION for all arrhythmias arising from a focal area eg WPW and others
The most common method for all arrhythmias except AF used today is to perform RF ablation.
Multiple randomised trials have shown that this technique is superior to drug therapy and therefore it is reasonable to use this as the gold standard to judge other therapies and techniques by.
Alternative approaches have focused on using alternative energy sources, or technologies to make delivery of the point-by-point RF easier in the case of AF.


